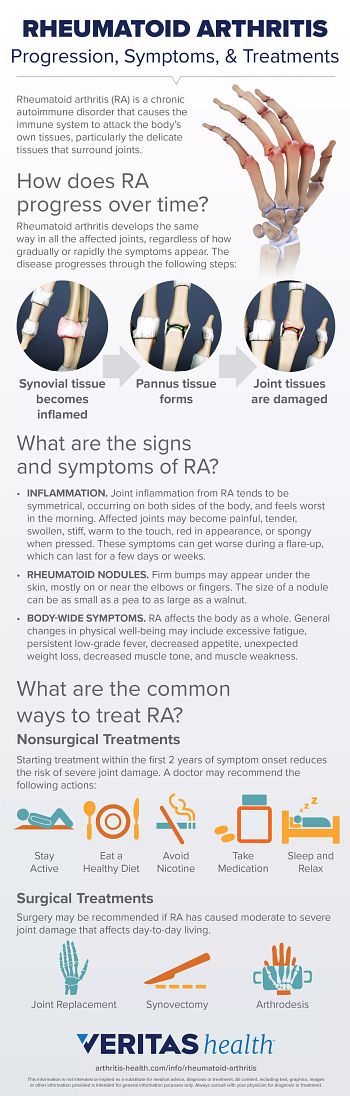
RA inflammation affects more than joints. The signs and symptoms of RA and conditions related to it may be felt all over the body, including in the ears, eyes, skin, lungs, and heart. Below is a description of 9 unusual symptoms that may be related to your rheumatoid arthritis.
Rheumatoid arthritis is an autoimmune disease that causes painful swelling, stiffness, and deformities of the joints. Watch: Rheumatoid Arthritis Overview Video
1. Hearing problems
Researchers have found that hearing loss and tinnitus (constant ringing, buzzing, or whistling in the ears) can be linked to rheumatoid arthritis. Hearing problems typically show up in older people who have had rheumatoid arthritis for many years.
Experts suggest many ways RA may contribute to hearing problems:
- Rheumatoid arthritis inflammation may damage the tiny joints in the ear.1
- A rheumatoid nodule can develop inside the ear.1
- Drugs that reduce RA symptoms, including aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs)2 and hydroxychloroquine3, may occasionally bring on tinnitus and/or hearing loss.
- Other disease processes may affect the auditory nerves or cochlear hair cells in the ear that are necessary for hearing.1
Some hearing problems are treatable—for example, stopping the use of NSAIDs may reverse symptoms—while others may be permanent. Even when changes to hearing are permanent, steps may be taken to stop or slow down future hearing loss.
Rheumatoid Arthritis
(larger view)
2. Snoring
Research suggests a significant connection between rheumatoid arthritis and sleep apnea4,5, which causes breathing to repeatedly stop and start during sleep. Symptoms include loud snoring and interruptions in breathing and/or gasping for breath while sleeping.
Sleep apnea can also cause headaches and contribute to chronic fatigue because the body takes in less oxygen at night.
Sleep apnea can be diagnosed and treated. Treatment typically includes using a continuous positive airway pressure (CPAP) machine or another treatment device to increase oxygen intake while sleeping.
3. Skin rash
When RA inflammation affects the blood vessels (Rheumatoid Vasculitis / Vasculitis), it can cause a variety of problems, including skin rashes. These rashes may appear as clusters of dark red or purple bumps, hives, or irregularly shaped raised pink patches on the skin. On darker skin, changes in skin color may be less noticeable.
Rashes related to vasculitis can occur anywhere but are most common on the lower legs. Sometimes these rashes are itchy, painful, or burning.
In addition, biologics medications used to treat RA increase the risk of rashes and other skin problems6, such as skin infections.
If you have a persistent rash that has lasted for more than 2 weeks, is painful, or looks infected, it’s advisable to contact your physician. Medical treatment is recommended for any rash that is persistent, severe, or accompanies symptoms of vasculitis in other areas of the body, such as the lungs, heart, kidneys, or eyes.
4. Trouble breathing, chronic cough, or chest pains
The lungs are commonly affected by rheumatoid arthritis, especially if the RA is long-standing and has not been well-managed.
Shortness of breath accompanied by a chronic cough, fatigue, and/or weakness may be a sign of scarring caused by chronic inflammation of the lungs. Shortness of breath accompanied by fever and/or chest pain when breathing may be a sign of fluid build-up around the lungs (pleural effusion). Both lung scarring and pleural effusion can be serious conditions, and medical attention is recommended.
5. Sudden, temporary numbness in the fingers or toes
Rheumatoid arthritis increases the risk for Raynaud Syndrome, also known as Raynaud Phenomenon or Raynaud disease. This condition causes one or more fingers or toes to lose blood circulation. The affected area will feel numb and appear paler, white, or blueish. There is typically a distinct border between this area and normal-colored tissue.
Raynaud Syndrome can be triggered by cold exposure, emotions, and certain medications.7 An episode may last minutes or hours. A warm compress, bath, or shower may encourage blood flow. If symptoms do not resolve then medical intervention may be necessary to prevent tissue damage.
6. Gum disease
Rheumatoid arthritis is associated with gum inflammation (gingivitis) and gum disease (periodontitis).8,9 Both of these conditions are linked to worsening RA symptoms10 and can lead to gum damage and tooth loss.
Regular dental checkups and good oral hygiene at home may help improve oral health as well as ease rheumatoid arthritis symptoms, such as joint tenderness and swelling.11,12,13
7. Increased fat-to-lean mass ratio
People who have RA tend to have a higher fat-to-lean mass ratio than people who do not have RA.14,15 This difference tends to hold true even for people whose weights are within normal range. Experts are not sure why.
Strengthening exercises can help counteract the loss of muscle. If applicable, losing excess weight may decrease rheumatoid arthritis disease activity and therefore reduce symptoms.16 The combination of building muscles and losing excess weight will support joint health and may reduce RA symptoms.
8. Red eyes
While nearly everyone experiences temporarily irritated, red eyes occasionally, eye redness that is recurring, persistent, and/or severe may be a sign of a medical condition related to RA. Eye conditions may be temporary or life-long and typically cause other symptoms, such as eye pain, sensitivity to light, watering, or irritation.
Signs and symptoms of eye problems, including any changes in vision, should be immediately reported to a health care practitioner.
9. Numbness or tingling
A damaged or pinched nerve can cause numbness and tingling in the hands, feet, or other areas of the body. Rheumatoid arthritis may contribute to nerve injury in a few ways:
- Swollen joint tissues cause a nerve to be pinched (for example, carpal tunnel syndrome can result from swollen joints in the wrist)
- Vasculitis related to RA affects blood flow and causes nerve damage
- Certain RA medications may also cause side effects of numbness and tingling sensations
While not necessarily painful, it’s best to report sensations of numbness and tingling to a physician. Addressing the cause may help prevent nerve problems from becoming worse or chronic.
New and unusual symptoms are not always related to rheumatoid arthritis. Contact your doctor to identify the possible cause of unfamiliar symptoms and discuss treatment strategies.